By: Thalia Kaylyn Averil
Transcranial Magnetic Stimulation (TMS) is a technique used to stimulate nerve cells in the brain using a magnetic field. This procedure is referred to as a non-invasive procedure because it does not use incisions on the skin. TMS is commonly used as supportive treatment, meaning it is a form of treatment conducted to help alleviate symptoms of the underlying condition. This can be administered while the patient is undergoing primary treatment. Transcranial magnetic stimulation is commonly used to treat strokes and migraines. TMS, especially repetitive TMS (rtMS), can play a role in stroke therapy because TMS can influence brain activity patterns. After a patient experiences a stroke, there is a disruption in the balance of brain activity between the affected and unaffected area of the brain. TMS aims to overcome this imbalance by increasing activity in the part of the brain affected by the stroke. In migraine treatment, TMS plays a role in controlling hyperactive nerve cells in the brain so that it can reduce the pain experienced by patients.
Apart from that, TMS can also be used for other diseases treatment, such as:
- Major depressive disorder
- Obsessive Compulsive Disorder (OCD)
- Quitting smoking or other addictions
- Alzheimer’s disease
- Bipolar disorder
- Borderline Personality Disorder (BPD)
- Chronic pain
- Eating disorders
- Tremors
- Fibromyalgia
- Parkinson’s disease
- Post-Traumatic Stress Disorder (PTSD)
- Schizophrenia
- Tinnitus
- Traumatic brain injury
Electricity and magnetism are two basic physics concepts that work together to underlie the mechanism of transcranial magnetic stimulation. Magnets can produce a magnetic field, which is the space around the magnet that is magnetically active. Electricity is produced when a magnet is brought close to a conductive object due to the interaction between the object and the magnetic field. On the other hand, the brain is electrically active, which means that small electrical currents are used by neurons or nerve cells in the brain and nerves throughout the body to send and receive information between the body’s organs. This electrical activity of the brain can be changed by placing a magnet nearby. TMS will change its magnetic field quickly to induce electrical currents to the superficial layers of the cerebral cortex in the brain that are associated with the disease to be treated.

Figure 1. Transcranial magnetic stimulation device.
- Tesla (T) is a unit used to measure magnetic strength. The majority of TMS magnets produce magnetic fields between 1.5T and 2T, which is comparable to the magnetic fields produced by MRI. However, the magnet used for TMS is much smaller than the magnet for MRI so the TMS magnetic field is also much smaller.
- Each time the magnetic field turns on and off, a pulsation is formed. Frequency (measured in hertz/Hz) is the number of pulses per second. TMS can use high frequency pulses at 5 Hz to 10 Hz or low frequency pulses at 1 Hz. This frequency influences the effects caused by TMS, low frequencies will have inhibitory effects, while high frequencies will have excitatory effects. Repetitive Transcranial Magnetic Stimulation (rTMS) is TMS that uses repeated pulses.
- Different pulse patterns can also be used by TMS for therapeutic purposes, such as Theta Burst Stimulation (TBS). Three bursts of 5 Hz occurred during TBS for a total of fifteen pulses in one second. Treatment is completed five or six times faster when using TBS than when using other techniques.
- Different brain structures can be targeted by different types of magnetic coils. Deep TMS (dTMS) using an H-shaped helmet coil will target deeper brain structures than rTMS and TBS. Studies show that dTMS is useful in the treatment of Obsessive Compulsive Disorder or OCD.
Before undergoing TMS, patients should remove metal jewelry or glasses that they are currently wearing. Apart from that, it is also important to pay attention to patients who have metal implants in their bodies because the magnets used in TMS can attract the implants, causing pain to the patient or damage to the device. After that, the patient will be directed to sit in a chair located next to or below the magnet. Patients will be given earplugs or head protection because the magnetic sound produced by TMS is quite loud. The healthcare professional will stimulate the scalp with a single pulse to help determine the ideal location before starting treatment. The strength of the pulse will be increased gradually, the patient may feel a sensation like tapping from a magnet. TMS can last for approximately 30 minutes to 1 hour per patient.
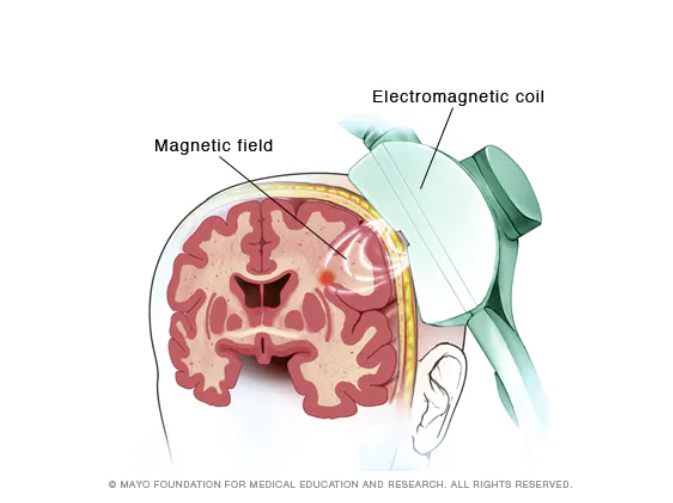
Figure 2. Transcranial magnetic stimulation.
So, what are the advantages of therapy using transcranial magnetic stimulation? Let’s explore more!
- TMS is a non-invasive procedure, which means that no anesthesia or surgery is performed on the patient. Therefore, patients can go home immediately and resume their normal activities after therapy
- TMS very rarely causes side effects in patients
- The success rate of TMS varies depending on the patient’s condition, but the effectiveness of TMS is very high according to current studies
- TMS can be used in conjunction with other therapies to achieve maximum results
Resources
- Chail A, Saini RK, Bhat PS, Srivastava K, Chauhan V. Transcranial magnetic stimulation: A review of its evolution and current applications. Ind Psychiatry J. 2018 Jul-Dec;27(2):172-180. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6592198/
- Cleveland Clinic. TMS (transcranial magnetic stimulation) [Internet]. Cleveland: Cleveland Clinic; date of publication unknown [reviewed 2022 Aug 29] [cited 2023 Des 10]. Available from: https://my.clevelandclinic.org/health/treatments/17827-transcranial-magnetic-stimulation-tms
- Mayo Clinic. Transcranial magnetic stimulation [Internet]. Rochester: Mayo Clinic; 2023 Apr 7 [cited 2023 Des 10]. Available from: https://www.mayoclinic.org/tests-procedures/transcranial-magnetic-stimulation/about/pac-20384625
- Fisicaro F, Lanza G, Grasso AA, Pennisi G, Bella R, Paulus W, Pennisi M. Repetitive transcranial magnetic stimulation in stroke rehabilitation: review of the current evidence and pitfalls. Ther Adv Neurol Disord. 2019 Sep 25;12:1756286419878317. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6763938/
