By: Thalia Kaylyn Averil
Inflammatory Bowel Disease (IBD) is a group of diseases characterized by inflammation of the digestive tract. IBD occurs due to repeated inflammatory processes in the intestines which are triggered by an abnormal immune response to bacteria that normally reside in the digestive tract. IBD can be divided into three types based on the localization and depth of involvement in the intestinal wall, namely ulcerative colitis, Crohn’s disease, and indeterminate colitis if it is difficult to differentiate between ulcerative colitis and Crohn’s disease. In ulcerative colitis, there is inflammation that spreads diffusely in the mucosa of the colon or large intestine. Ulcerative colitis generally occurs in the rectum and can progress to the upper part, such as sigmoid (the end of the large intestine) or even to cecum (the beginning of the large intestine) which is characterized by pancolitis, which is inflammation that occurs in all parts of the large intestine. On the other hand, Crohn’s disease can cause ulceration of the entire digestive tract. However, this disease most often occurs in the terminal ileum (the final part of the small intestine) and the large intestine.
The intestinal immune system plays an important role in causing IBD. The intestinal lining acts as a protector that can prevent harmful substances, such as bacteria or antigens, from entering the bloodstream. In patients with IBD, this protective system is weakened by severe inflammation and cannot function properly. The body also has another defense system, including mucus produced by cells in the digestive tract and the release of antimicrobial substances. However, excessive inflammatory reactions cause the intestinal lining to become increasingly damaged, coupled with exposure to intestinal microbes which can worsen inflammation.
In ulcerative colitis, there is continuous inflammation in the layers of the large intestine and rectum, leading to swelling, ulcers, bleeding, and loss of electrolytes. On the other hand, Crohn’s disease can attack any part of the digestive tract, causing narrowing, inflammation or abnormal formation of the tract. If this disease becomes chronic, the large intestine can become stiff and shortened, losing its normal appearance. Ulcerative colitis can cause problems in other organs besides the intestine, such as skin, eye, and bone problems. On the other hand, Crohn’s disease mostly affects the large intestine, but can also involve other parts. Both conditions can lead to complications such as inflammation in the joints and eyes. In ulcerative colitis, there is a higher risk of kidney disease and gallstones due to poor absorption of certain substances.
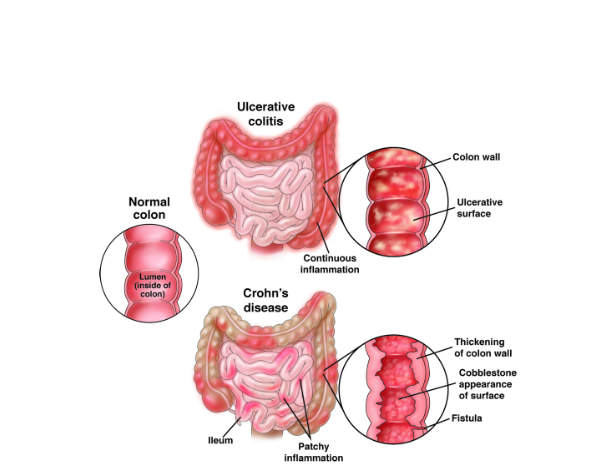
Figure 1. Ulcerative colitis and Crohn’s disease.
IBD often appears as chronic diarrhea, with or without blood, accompanied by abdominal pain. Patients with IBD may also experience problems beside the gut. IBD can be divided into two phases, which are the remission phase and the active phase. The remission phase is caused by treatment or recovery that occurs spontaneously. In ulcerative colitis, symptoms can start with severe symptoms or mild symptoms that get worse gradually. The severity is often influenced by which part of the colon is affected. In Crohn’s disease, apart from the general symptoms, the presence of fistulas or abnormal ducts is the main characteristic. Abdominal pain will be more pronounced in patients with Crohn’s disease because the lesions affect all parts of the intestinal wall, which can cause fistulas, blockages and excessive bacterial growth.
Diagnosis of IBD can be done with the following steps:
- Medical history is very useful in diagnosing IBD, such as whether there is recurrent diarrhea, diarrhea that is accompanied by blood, or abdominal pain. Apart from that, it is also important to know the family history of the disease.
- Healthcare workers will also carry out a physical examination of general condition, nutritional status, and tenderness in the stomach.
- Laboratory examination serves to rule out other causes of inflammation, especially gastrointestinal infections which are common in Indonesia. In addition, it is also important to exclude tuberculosis because the symptoms are similar to Crohn’s disease. Laboratory tests that can be carried out are complete blood tests, feces, erythrocyte sedimentation rate as a marker of inflammation, and C-reactive protein, which is a protein produced by the liver as a response to inflammation. Gastrointestinal pathogen panel is an example of a stool examination that can be carried out to detect microorganisms that cause infections in the digestive tract.
- Endoscopy, pathology and radiology examinations can also be carried out as a way to diagnose IBD. Radiological examinations can include plain abdominal radiographs, double contrast barium, CT scans, and ultrasound. Endoscopic examination plays an important role in diagnosing IBD with a diagnostic accuracy of 89%. Endoscopy can be performed for early detection of IBD, enabling patients to receive timely treatment, potentially improving the prognosis of IBD patients.
- Healthcare workers will monitor the patient’s condition from time to time.
Resources
- Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo PL, Jameson JL. Harrison’s principles of internal medicine. 19th ed. New York: McGraw-Hill; 2015.
- Setiati S, Alwi I, Sudoyo AW, Simadibrata M, Setiyohadi B, Syam AF, editor. Buku ajar ilmu penyakit dalam. 6th ed. Jakarta: Interna Publishing; 2014.
- McDowell C, Farooq U, Haseeb M. Inflammatory Bowel Disease. [Updated 2023 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470312/
- American Gastroenterological Association. Inflammatory bowel disease (IBD) [Internet]. Bethesda: AGA GI Patient Center; date of publication unknown [cited 2024 Apr 5]. Available from: https://patient.gastro.org/inflammatory-bowel-disease-ibd/
