By: Thalia Kaylyn Averil
Hemorrhoids are enlarged and swollen blood vessels that form inside or outside the rectum and anus, causing pain, discomfort and bleeding. Initially, hemorrhoidal cushions are normal anatomical structures that contain blood vessels and can be found in the anal canal. However, hemorrhoid pads can become swollen and stretched, resulting in prolapse of the tissue.Over time, the support system of these structures weakens, causing the tissue to protrude from the anal canal and become more susceptible to injury. This disease affects individuals of all ages and genders, but increasing age can increase the risk of developing hemorrhoids.Hemorrhoids can also be influenced by an unhealthy diet, such as frequently consuming low-fiber, high-fat foods. Hemorrhoids can be classified based on their location.
- External hemorrhoids: Hemorrhoids that form inside the anus. Patients with external hemorrhoids may experience itching, pain, and sometimes bleeding.
- Internal hemorrhoids: Hemorrhoids that form inside the rectum or the part of the digestive system that connects the large intestine to the anus. In general, internal hemorrhoids cause bleeding, but do not cause pain.
- Prolapsed hemorrhoids: External and internal hemorrhoids can prolapse, protruding outside the anus. This can cause bleeding or pain.
Hemorrhoids can also be classified based on their progression from their normal internal position to their prolapsed external position. This classification will also determine the appropriate treatment for the patient.
- Stage 1: Hemorrhoids enlarge and may bleed. Treatment options include fiber supplementation, cortisone suppositories, and sclerotherapy.
- Stage 2: Hemorrhoids protrude and can reduce on their own. Treatment options include fiber supplementation and cortisone suppositories.
- Stage 3: Hemorrhoids protrude and require manual reduction. Treatment options include fiber supplementation, cortisone suppositories, ligation, and operative hemorrhoidectomy.
- Stage 4: Hemorrhoids cannot be reduced. Treatment options include fiber supplementation, cortisone suppositories, and operative hemorrhoidectomy.
There is no best treatment for hemorrhoids because each patient’s needs are different. In addition to hemorrhoid classification, treatment options are also based on a thorough history and physical examination performed by a doctor. The effectiveness of each treatment may vary depending on the severity of the lesion and other factors.
- Rubber band ligation
- Ligation is one method of treating hemorrhoids using a small instrument called a ligator and rubber band. The ligator is inserted through a tube called a scope into the anal canal. Then, the doctor will hold the hemorrhoid with forceps and slide the ligator upwards to remove the rubber band right around the base of the hemorrhoid. This rubber band will cut off the blood supply to the hemorrhoids resulting in necrosis (death of the cells in the hemorrhoids) which leads to the hemorrhoids decreasing in size and then falling off. The advantage of this method is that it causes little pain and can be used to treat recurring hemorrhoids.
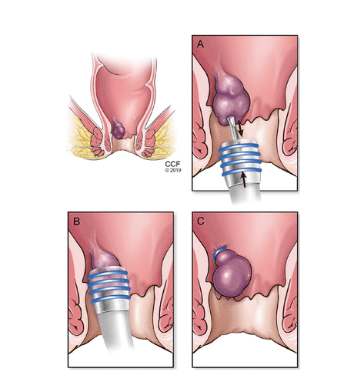
Figure 1. Rubber band ligation
- Sclerotherapy
Sclerotherapy is a procedure that involves injecting a sclerosing agent into the hemorrhoid, which causes an inflammatory reaction that eventually forms fibrotic tissue, cutting off blood flow to the hemorrhoid. Sclerotic agents that can be used are 5% phenol in almond oil or vegetable oil, quinine, ethanolamine, and hypertonic salt solution. After undergoing this therapy, patients may experience pain and fever.
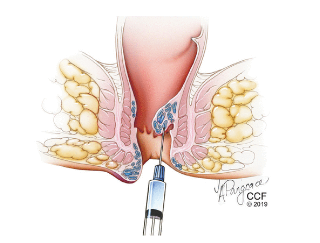
Figure 2. Sclerotherapy.
- Stapled hemorrhoidopexy
In this procedure, the prolapsed hemorrhoid tissue will be repositioned by connecting it to the rectal wall located directly above the hemorrhoid. First, a special tool is inserted into the anal canal, then the excess tissue is cut and removed, then the remaining tissue is pulled to its normal position. This method causes less pain than other surgical procedures for hemorrhoids.
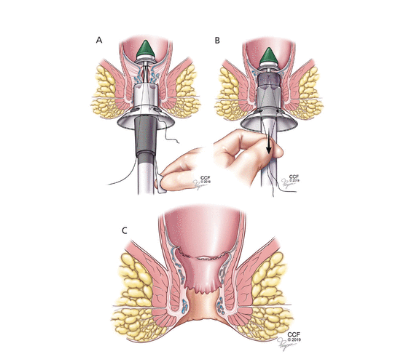
Figure 3. Stapled hemorrhoidopexy.
- Laser hemorrhoidoplasty
Laser hemorrhoidoplasty is a minimally invasive procedure used to treat hemorrhoids. To identify the arteries to be targeted, doctors may use a transducer that will be inserted into the rectum. Once the artery is found, doctors will insert a laser probe into the hemorrhoid, then this laser targets hemoglobin (protein inside the red blood cells) and closes the artery around the hemorrhoid. Lasers can cut off the blood supply to hemorrhoids causing the surrounding tissue to shrink. This method can minimize the risk of bleeding during and after the procedure. A study found that laser hemorrhoidoplasty resulted in low levels of postoperative pain and reduced recurrence rates in the long term.
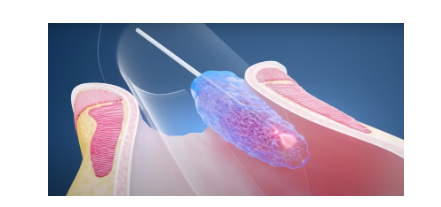
Figure 4. Laser hemorrhoidoplasty.
Resources
- Cleveland Clinic. Hemorrhoids [Internet]. Cleveland: Cleveland Clinic; date of publication unknown [reviewed 2021 Jan 18] [cited 2024 May 28]. Available from: https://my.clevelandclinic.org/health/diseases/15120-hemorrhoids
- Longo DL, Fauci AS, Kasper DL, Braunwald E, Hauser SL, Jameson JL, Loscalzo J. Harrison’s gastroenterology and hepatology. 17th ed. New York: McGraw-Hill; 2010.
- Cengiz TB, Gorgun E. Hemorrhoids: a range of treatments. CCJM. 2019 Sep;86(9):612-20. doi: 10.3949/ccjm.86a.18079. Available from: https://www.ccjm.org/content/86/9/612
- IBI Healthcare. Laser hemorrhoidoplasty (LHP) – IBI Healthcare Institute [YouTube video]. Georgia: IBI Healthcare; 2023 Jan 25. Available from: https://youtu.be/o3YhMZIvx3s?si=2bmslz5ZyIh4neqa
- Torrinha G, Goncalves T, Sousa M, Hogemann G, Goulart A, Carvalho AF, Leao P. The effects of laser procedure in symptomatic patients with haemorrhoids: a systematic review. Frontiers. 2022 Dec 12;9. doi: 10.3389/fsurg.2022.1050515. Available from: https://www.frontiersin.org/articles/10.3389/fsurg.2022.1050515/full
