Oleh: Thalia Kaylyn Averil
Penyakit Alzheimer adalah penyebab paling umum dari demensia dan jenis demensia yang paling umum dijumpai pada lansia. Alzheimer yang telah berkembang dapat menyebabkan penderitanya kehilangan kemampuan kognitif secara progresif, seperti ingatan, penilaian, kepribadian, orientasi visuospasial, dan bahasa. Penderita Alzheimer sering kali mengalami kecacatan, kebisuan, dan imobilitas yang parah dalam jangka waktu lima hingga sepuluh tahun.
Penyakit ini telah dikaitkan dengan sejumlah faktor risiko. Faktor risiko terbesarnya adalah usia, Alzheimer biasanya tidak menunjukkan gejala sampai pasien telah mencapai usia 50 tahun. Peluang untuk terkena penyakit ini meningkat secara drastis seiring bertambahnya usia, prevalensi Alzheimer meningkat dua kali lipat setiap lima tahun, dimulai dari 1% pada kelompok usia 60–64 tahun dan meningkat menjadi 40% atau lebih tinggi pada kelompok usia 85–89 tahun. Namun, demensia dini dapat terjadi jika seseorang mengalami trisomi 21, salah satu penyebab down syndrome. Selain itu, faktor risiko lain dari Alzheimer termasuk cedera otak traumatis, depresi, penyakit kardiovaskular, penyakit serebrovaskular, kebiasaan merokok, riwayat demensia dalam keluarga, peningkatan kadar homosistein, dan keberadaan alel APOE e4.
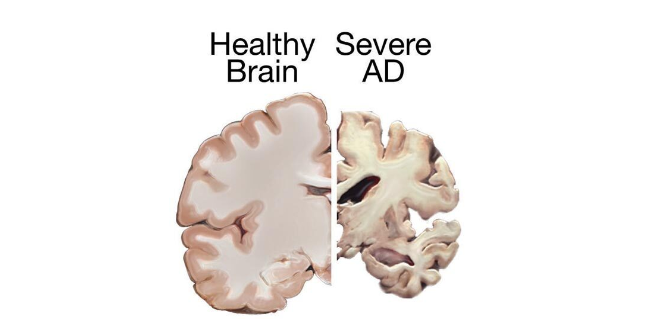
Gambar 1. Gambaran otak normal (kiri) dan otak pada penderita Alzheimer (kanan).
Ciri patologis dari penyakit Alzheimer adalah plak amiloid dan gumpalan neurofibriler, keduanya terutama terlihat pada tahap akhir penyakit. Plak amiloid adalah penumpukan peptida beta-amyloid (Aβ) pada materi abu-abu di otak, sementara gumpalan saraf neurofibriler adalah akumulasi protein tau yang biasanya terjadi di dalam sel saraf. Alzheimer disebabkan oleh adanya kematian neuron dan biasanya dimulai dari salah satu wilayah di otak, yaitu korteks entorhinal.
- Plak amiloid: Timbunan peptida beta-amiloid ekstraseluler akan terbentuk menjadi plak neuritik sehingga terlihat lesi mikroskopis berbentuk bulat. Sebuah hipotesis menyatakan bahwa penumpukan beta-amiloid di otak dapat memicu hilangnya koneksi antar sel saraf dan kekurangan neurotransmitter atau zat pengirim pesan di otak yang kemudian berkontribusi pada munculnya gejala demensia.
- Gumpalan neurofibriler: Gumpalan neurofibriler adalah kumpulan benang-benang yang terbentuk di dalam sel otak dan terbuat dari penumpukan protein tau yang tidak normal. Pada normalnya, protein tau membantu sel otak dengan transportasi internalnya. Namun, protein tau mengalami perubahan bentuk dan membentuk gumpalan neurofibriler pada penyakit Alzheimer. Hal ini menyebabkan gangguan pada sistem transportasi di dalam sel otak dan merusak sel-sel tersebut.
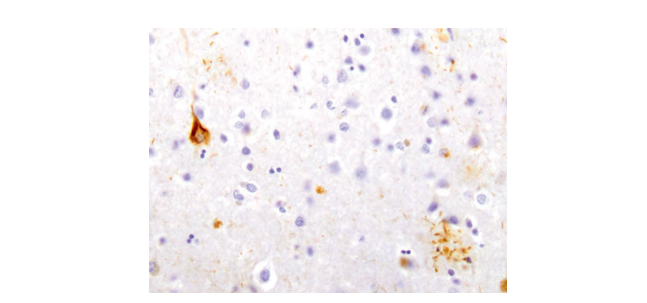
Gambar 2. Plak amiloid (kanan bawah) dan gumpalan saraf neurofibriler (kiri atas).
Selama beberapa tahun, gejala penyakit Alzheimer berkembang secara bertahap. Penyakit ini dapat dibagi menjadi tiga tahap, yaitu tahap awal, tahap tengah, dan tahap akhir. Hilangnya ingatan adalah tanda utama penyakit Alzheimer pada tahap awal. Pada tahap awal, biasanya seseorang dengan Alzheimer akan mengalami hal berikut:
- Melupakan kejadian yang baru-baru ini terjadi atau letak benda
- Menanyakan pertanyaan yang sama berulang kali
- Sulit mengambil keputusan
- Menjadi kurang mudah beradaptasi dan lebih berhati-hati ketika mencoba hal baru
- Perubahan suasana hati, sering kali ditandai dengan meningkatnya kecemasan atau kegelisahan
Perkembangan penyakit Alzheimer akan memperburuk masalah memori. Seseorang yang menderita penyakit ini mungkin akan semakin sulit mengingat nama orang yang mereka kenal, seperti keluarga, teman, tetangga, dan lain-lain. Biasanya, penderita Alzheimer pada tahap ini memerlukan bantuan dalam melakukan kegiatan sehari-hari. Selain itu, tanda dan gejala berikut juga dapat muncul pada tahap tengah:
- Munculnya disorientasi, seperti tersesat atau berkeliaran tanpa mengetahui waktu
- Delusi atau memiliki kecurigaan terhadap orang-orang terdekat
- Bermasalah dengan bahasa atau ucapan
- Munculnya halusinasi
- Kecemasan dan kegelisahan semakin sering terjadi
Pada tahap akhir, hal-hal yang sering dialami oleh penderita Alzheimer adalah delusi dan halusinasi yang semakin memburuk seiring berjalannya waktu serta menunjukkan perilaku kekerasan, menuntut, dan tidak percaya terhadap orang lain di sekitarnya. Ketika penyakit Alzheimer memburuk, sejumlah gejala tambahan juga bisa muncul, termasuk:
- Disfagia atau kesulitan menelan dan makan
- Kesulitan bergerak atau berpindah posisi sendiri
- Penurunan berat badan
- Inkontinensia, yaitu hilangnya kontrol akan kandung kemih sehingga sulit untuk menahan buang air kecil
- Hilangnya suara secara progresif
Lalu, apa saja yang dapat dilakukan untuk mencegah terjadinya penyakit Alzheimer?
- Kendalikan dan cegah tekanan darah tinggi
Selain menurunkan risiko penyakit jantung dan stroke, mengendalikan tekanan darah tinggi juga dapat membantu mencegah penyakit Alzheimer. Tekanan darah tinggi adalah salah satu faktor risiko penurunan kognitif pada lansia.
- Lakukan aktivitas fisik secara teratur
Manfaat dari aktivitas fisik adalah menurunkan risiko jatuh, menjaga mobilitas, menjaga berat badan ideal, dan meningkatkan kesehatan jantung. Hal ini dapat mengurangi risiko terjadinya stroke, tekanan darah tinggi, diabetes, depresi, dan penyakit lain yang dapat memperburuk penurunan kognitif terkait usia.
- Berhenti merokok
Berhenti merokok dapat menurunkan risiko penyakit paru-paru, kanker, penyakit jantung, dan penyakit lain yang berhubungan dengan rokok serta menjaga kesehatan otak.
- Kontrol gula darah
Pelajari cara mengelola gula darah untuk penderita diabetes.
- Konsultasikan ke dokter
Jika Anda memiliki faktor risiko, terutama jika sudah lansia, atau mengalami tanda dan gejala penyakit Alzheimer di atas, segera konsultasikan ke dokter untuk mendapatkan pemeriksaan lebih lanjut. Pada Alzheimer, pemindaian MRI bermanfaat untuk mengidentifikasi tanda-tanda awal penyakit Alzheimer dan membedakan penyebabnya yang penting untuk diagnosis dini dan memulai pengobatan dini. Pemindaian MRI dapat mendeteksi perubahan spesifik pada otak pasien penyakit Alzheimer. Salah satunya adalah atrofi atau bagian otak yang terkait dengan penyakit ini tampak mengecil, seperti di hipokampus, korteks entorhinal, dan lain-lain. Selain itu, hiperintensitas materi putih di otak yang menunjukkan demielinasi dan hilangnya aksonal juga terlihat.
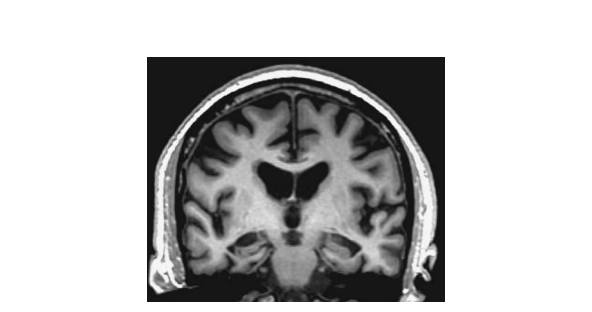
Gambar 3. MRI pada penderita Alzheimer.
Referensi:
- Ropper AH, Samuels MA, Klein JP, Prasad S.Adams and victor’s principles of neurology. 11th ed. New York: McGraw Hill; 2019.
- Kumar A, Sidhu J, Goyal A, Tsao JW. Alzheimer disease [Internet]. Unknown ed. Treasure Island: StatPearls Publishing; date of publication unknown [updated 2022 Jun 5] [cited 2024 Jan 31]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499922/
- National Health Service. Overview – Alzheimer’s disease [Internet]. England: National Health Service; date of publication unknown [reviewed 2021 Jul 5] [cited 2024 Jan 31]. Available from: https://www.nhs.uk/conditions/alzheimers-disease/
- Johnson KA, Fox NC, Sperling RA, Klunk WE. Brain imaging in Alzheimer disease. Cold Spring Harb Perspect Med. 2012 Apr;2(4):a006213. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3312396/
